

Connected by Hearts is a community that provides education, support, and networking to young sudden cardiac arrest survivors and those living with a heart condition. We all took our own path to get here but we can continue the journey Connected by Hearts.
Connect on Discord
- Share your story
- Ask questions
- Chat and connect with people who can understand your situation
- See updates about medical and legal advances related to SCA

Why Connect?
We all come to Connected by Hearts from different places. Many of us have experienced a sudden cardiac arrest (SCA), while others were diagnosed with heart issues prior to having an event. Some of us still don’t have a specific diagnosis. Several of us are living with an implantable cardioverter defibrillator (ICD) or pacemaker.
Because of your condition you might have had to make lifestyle changes that have impacted your school experience, team activity or relationships. Maybe you’re sad, mad or scared about what happens next. Whatever our story, we all share some commonalities. Our lives can be challenging but we know we can gather strength and compassion from each other.
We welcome you to connect with this community through Discord, whether it’s your story, or it’s your friend or sibling who has been affected, feel free to ask questions and reach out to us. We will provide answers to the best of our ability, with the opportunity to connect with people who can understand your personal situation.
News
-
 Nurse driving by group of boys stops and saves 17-year-old as he suffers heart attack
Nurse driving by group of boys stops and saves 17-year-old as he suffers heart attack
-
 More defibrillator stations installed in Sonoma
More defibrillator stations installed in Sonoma
-
 School staff save West Michigan 1st grader from cardiac arrest
School staff save West Michigan 1st grader from cardiac arrest
-
 Bleeding control, defibrillator equipment would be required in schools under proposed bill
Bleeding control, defibrillator equipment would be required in schools under proposed bill
-
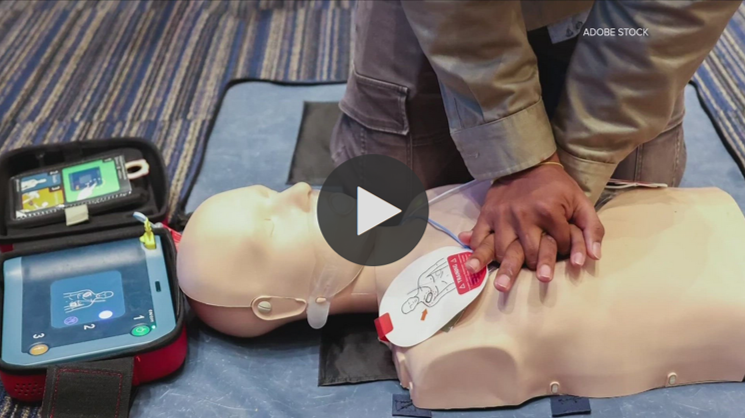
 VIDEO: Hillsborough deputies save high school student using CPR, defibrillator
VIDEO: Hillsborough deputies save high school student using CPR, defibrillator
-
 Valley pre-teen athlete says routine visit led to life-altering diagnosis
Valley pre-teen athlete says routine visit led to life-altering diagnosis
-
 Bayonne High School student welcomed home after collapsing in class from irregular heartbeat
Bayonne High School student welcomed home after collapsing in class from irregular heartbeat
-
 SC lawmakers propose a bill to reduce death due to cardiac arrest in schools
SC lawmakers propose a bill to reduce death due to cardiac arrest in schools
-
 Lawmakers to consider bill requiring AEDs in all Georgia schools
Lawmakers to consider bill requiring AEDs in all Georgia schools
-
 Over half of children with out-of-hospital cardiac arrest experience 1 adverse safety event
Over half of children with out-of-hospital cardiac arrest experience 1 adverse safety event
 5 Saves & Advances
5 Saves & Advances
in Prevention
BASED ON NEWS STORIES THIS YEAR,
AND ONLY A FRACTION OF ACTUAL EVENTS
Learn More About Your Heart Condition
What is Brugada Syndrome?
Brugada Syndrome is a genetic syndrome which can cause an abnormal electrical current in the heart. This abnormal electric current can lead to abnormal heartbeats which can affect the heart’s ability to pump blood.
What are the symptoms of Brugada syndrome?
Individuals with Brugada syndrome may not have any symptoms. If individuals do have symptoms they may include:
- Episodes of passing out
- Fast heartbeat
- Chest pain
- Changes in breathing at night
Individuals with Brugada syndrome are at a risk of going into a dangerous abnormal heart rhythm. Unfortunately, some people may have no symptoms before the heart goes into the abnormal rhythm. Patients should maintain regular visits to healthcare practitioners for follow-up.
How is Brugada Syndrome diagnosed?
An electrocardiogram (EKG or ECG) is used to detect an abnormal electrical current in the heart. There are classic changes on the EKG reading which would alert your physician to the possibility of Brugada syndrome.
Individuals with Brugada syndrome should let their physician know if they have anyone in their family who has had heart problems at a young age.
How is Brugada Syndrome Treated?
There are a variety of treatments for Brugada syndrome. One important treatment is the Implantable Cardioverter-Defibrillator (ICD) which can identify and correct abnormal electric currents in the heart through an electric shock. If patients are unable to get the ICD placed or do not wish to have an ICD, then there are certain medications that can be given. These medications act to prevent the heart from going into the abnormal rhythm.
Since Brugada syndrome runs in families, it is important to test other members of the family for this condition.
BRUGADA SYNDROME: IMPORTANT TERMINOLOGY
Genetic Syndrome: A condition that runs in families. This may be present in a variety of patterns. It is not necessary that one’s parents have to show a disease for it to be passed on.
Electrocardiogram (EKG or ECG): An electrocardiogram is a test that measures the electrical activity in the heart. A number of electrodes (stickers) are put on the skin on the upper chest, arms, and legs. These are then connected to a monitor that records a snapshot or picture of how the heart is pumping. This test is used to look for any abnormal electrical activity in the heart. Watch
Implantable Cardioverter Defibrillator (ICD): The ICD is a device put under your skin which tracks your heartbeat and can deliver a shock to correct the heartbeat.
What is HCM?
Hypertrophic Cardiomyopathy is a condition that causes a thickening of the heart muscle causing it to become too bulky. The hypertrophy or growth can become so significant that it interferes with how the heart pumps. HCM is the most common cardiomyopathy and occurs in about 1 in 300 individuals. HCM runs in families and specific genetic mutations having been identified that are linked to HCM. The vast majority of people with HCM live long and healthy lives. Most individuals with HCM don’t even show symptoms. However, a small number of individuals with HCM are at increased risk for a serious complication due to heart failure. This risk is particularly high in young people with this condition. Watch
What are the symptoms of HCM?
Most people with HCM do not have any symptoms of the disease. However, it is important for both family members and healthcare providers to recognize the symptoms when they occur. Here are some common symptoms:
- Chest pain (particularly worse when exercising or after heavy meals)
- Shortness of breath (particularly worse when exercising or after heavy meals)
- Feeling tired (fatigue)
- Feeling of fluttering or fast heartbeats (palpitations)
- Lightheadedness
- Passing out spells (syncope)
- Swelling in your arms or legs (edema)
- Heart murmur (detected by doctor)
How is HCM diagnosed?
Since HCM runs in families, it is important to screen those individuals with family members who have the disease. A physician may suspect HCM if the individual has some of the symptoms listed above or if a family member has HCM, particularly at a young age. The goal of screening for HCM is:
- To determine whether the individual has HCM
- To determine the severity of HCM if it is present
The initial test done to diagnose HCM is an Electrocardiogram or EKG. This test looks for any abnormal electrical activity in the heart. Most individuals with HCM have abnormal electrical activity in the heart that shows up on the EKG. Some individuals may be asked to wear a Holter monitor (a portable version of the EKG) for 24-48 hours. Another test is a Trans-Thoracic Echocardiogram which looks at the structure of the heart. Individuals with HCM will have increased growth of their left ventricle (lower chamber). Some individuals will undergo a treadmill Exercise Stress Test. This test looks at how the heart responds to exercise.
The results from these tests along with the description of an individual’s symptoms and the clinical evaluation will help the physician determine whether the individual has HCM and to what severity. HCM runs in families, so it’s important to screen family members of those who have HCM.
How is HCM Treated?
The risk of serious complications (sudden death) among individuals with HCM is due to the overgrowth of the left ventricle (lower chamber). The left ventricle can grow so much that it blocks the ability of blood to leave the heart which makes it more difficult to pump the blood to the body. The treatment of HCM is directed towards preventing this scenario from occurring.
Physicians and patients can work together to ensure that individuals with HCM live long and healthy lives. Some possible therapies or treatments for HCM include:
- Avoiding dehydration
- Consulting a physician before increasing physical exertion or participation in competitive sports
- Screening close relatives of the individuals with HCM for HCM
- Taking medications to relieve chest pain or shortness of breath.
- Taking medicines to control the heart’s rhythm
- Undergoing surgery to implant a device called an implantable cardioverter-defibrillator, or ICD. (This device keeps the heart beating normally)
- Surgery or other treatments may be used to reduce the size of the left ventricle. (This is done only when medicines do not work)
What are some healthy lifestyle choices I can make if I am diagnosed with HCM?
Individuals with HCM should drink plenty of water to prevent dehydration and consult their physician for guidance on participation in competitive sports.
HCM: IMPORTANT TERMINOLOGY
Atrium (Atria pl): The upper chamber of the heart. There are two atria: left and right.
Cardiomyopathy: Cardiomyopathy is a long-term disease of the heart muscle (myocardium).
Echocardiogram: An echocardiogram is a type of ultrasound test that is used to look at the structure of the heart. The sonographer will move a transducer, with cool gel on it, across your chest and upper ribs. The transducer uses painless sound waves to look at the structure of the heart. Watch
Electrocardiogram (EKG or ECG): An electrocardiogram is a test that measures the electrical activity in the heart. A number of electrodes (stickers) are put on the skin on the upper chest, arms, and legs. These are then connected to a monitor that records a snapshot or picture of how the heart is pumping. This test is used to look for any abnormal electrical activity in the heart. Watch
Exercise Stress Test: The exercise stress test is done while the individual walks or runs on a treadmill while connected to the EKG machine (see EKG). The test determines how the heart responds to exercise. Watch
Genetic Mutation: A genetic mutation is a change in an individual’s DNA that can lead to improper functioning of their body’s cells. These mutations or changes may be passed down through generations. Watch
Hypertrophy: Hypertrophy is the increased growth of a tissue or organ (in this case the heart).
Implantable Cardioverter Defibrillator (ICD): The ICD is a device put under the skin that tracks the heartbeat and can deliver a shock to correct the heartbeat if an irregular heartbeat occurs.Watch
Ventricle: The lower chamber of the heart. There are two ventricles: left and right.
Pediatric Cardiomyopathies
In addition to Hypertrophic Cardiomyopathy (HCM), there are several other types of cardiomyopathies caused by abnormalities in the heart muscle, including Dilated Cardiomyopathy (DCM), Restrictive Cardiomyopathy (RCM), Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) and Left Ventricular Non-Compaction Cardiomyopathy (LVNC).
For more information, visit:
What is LV Non-compaction (LVNC)?
Left Ventricular Non-compaction is an uncommon congenital disease in which the left ventricle has an abnormal structure. This abnormal structure interferes with the way the heart beats and pumps blood. LVNC can run in families.
What are the symptoms of LV Non-compaction?
LV Non-compaction may be diagnosed by the initial symptoms of the patient. Some possible symptoms include:
- Shortness of breath
- Chest pain
- Feeling of heart racing
- Fainting
Some major complications of LVNC include:
- Stroke
- Heart Failure
- Irregular Heart Beat
How is LV Non-compaction diagnosed?
The diagnosis of LVNC focuses on identifying an abnormal structure of the left ventricle (the left bottom chamber of the heart). LVNC may be diagnosed by a physical exam, an abnormal electrocardiogram (EKG or ECG), or an abnormal echocardiogram.
How is LV Non-compaction treated?
The treatment for LVNC depends on the stage of disease and complications.
For possible heart failure, there are a number of medications that can help with the symptoms. For individuals who are at risk of having a stroke, blood thinning medications may be required. Individuals with LVNC are screened yearly for the presence of an abnormal heart beat.
Certain patients with LVNC may need to consult their physician for guidance on participation in exercise or high endurance sports. For patients with advanced disease, heart transplantation is an option for treatment. Family members of individuals with LVNC should be tested for the disease as it runs in families.
LVNC: IMPORTANT TERMINOLOGY
Atria (s. Atrium): The upper chambers of the heart. There are two atria: Left and Right.
Congenital: Any disease that has been present in an individual since birth.
Echocardiogram: An echocardiogram is a type of ultrasound test that is used to look at the structure of the heart. The sonographer will move a transducer, with cool gel on it, across your chest and upper ribs. The transducer uses painless sound waves to look at the structure of the heart. Watch
Electrocardiogram (EKG or ECG): An electrocardiogram is a test which measures the electrical activity in the heart. A number of electrodes (stickers) are put on the skin on your upper chest, arms, and legs. These are then connected to a monitor that records a snapshot or picture of how the heart is contracting. This test is used to look for any abnormal electrical activity in the heart. Watch
Ventricles (s. Ventricle): The lower chambers of the heart. There are two ventricles: left and right.
What are the Congenital Long QT Syndromes?
The heart is a muscle that contracts due to an electrical current that flows through it. This electrical current makes sure the heart beats with a regular rhythm. If there are changes to this electric current then the heart can beat with an abnormal rhythm. Congenital Long QT syndromes are a group of disorders that result in an abnormality in this electric current. This defect can cause the heart to go into a dangerous rhythm. Individuals are at risk of serious complications from this rhythm.
What are the Symptoms of Congenital Long QT Syndromes?
Many patients with Long QT will not have any symptoms of the disease. Some symptoms that can happen with Long QT syndromes are:
- Fainting (syncope)
- Feeling of fluttering or rapid heartbeats (palpitations)
- Lightheadedness
- Seizures or episodes which cause an individual to move or behave strangely
- Trouble hearing
How are the Congenital Long QT Syndromes Diagnosed?
The first step in diagnosing Long QT Syndromes is an Electrocardiogram or EKG. This test measures the electrical activity of the heart. Individuals with one of the Long QT Syndromes have specific irregularities on the EKG. An individual may be asked to wear a Holter monitor, which is a portable EKG monitor, for about 24-48 hours. This can monitor an individual’s heart rhythm for a longer period of time. The individual may undergo a treadmill Exercise Stress Test that determines how the heart responds to exercise.
Congenital Long QT Syndromes run in families. Individuals may require a blood test to see if they have the gene for the Long QT Syndromes. Because Long QT often runs in families, it is important to screen individuals with family members who have Long QT.
The results from these tests will help the physician determine whether an individual has a Long QT Syndrome and how severe the disease has become. Some specific names of Long QT syndromes include: Romano-Ward Syndrome and Lange-Nielsen Syndrome.
How are the Congenital Long QT Syndromes treated?
The focus of treatment for the Long QT Syndromes is to prevent the heart from going into an abnormal rhythm.
The treatment focuses on identifying and avoiding possible triggers for the abnormal rhythm. Possible triggers include: exercise; loud noises; emotional outbursts; and certain medications.
Medications for Long QT syndromes may include a beta-blocker which is a class of medication that slows down the heart rate. Some possible side effects of beta-blockers include: feeling tired, headache, upset stomach, constipation, dizziness, and shortness of breath.
Pacemakers or ICDs may be placed to monitor an individual’s heart beat and correct it if necessary.
In case the individual stops breathing or loses a pulse (Cardiac Arrest), Emergency Medical Services (EMS) should be notified. CPR should be performed, until the EMS arrives.
What lifestyle changes should I make if I am diagnosed with Long QT Syndrome?
Try to avoid the triggers that may cause the heart to go into an abnormal rhythm. Follow up regularly with your physician and follow their recommendations.
LONG QT SYNDROMES: IMPORTANT TERMINOLOGY
Arrhythmia: An arrhythmia is an abnormal heart beat. Some abnormal heartbeats are harmless while others can be dangerous. An arrhythmia is identified on an Electrocardiogram or EKG. Watch
Automated External Defibrillator (AED): An AED is a device that can detect life-threatening abnormal heart rhythms and can correct them by delivering an electric shock. If a life-threatening heart rhythm is present, the AED will deliver an electric shock to the individual. An AED is simple to use- just open the lid and the instructions will be read to you. The AED will not shock somebody if they have a normal pulse. AED devices should be used with care. It is important to make sure that noone else is touching the patient when the shock is delivered. Watch
Cardiopulmonary Resuscitation (CPR): CPR is needed when an individual is unresponsive and they don’t have pulse and/or they are not breathing. CPR can keep blood flowing to the brain and other important organs. CPR involves pushing hard and fast on the center of the chest until medical personnel arrives or an automated external defibrillator (AED) is available. Watch
Congenital: A congenital condition is a condition that an individual has since birth.
Electrocardiogram (EKG or ECG): An electrocardiogram is a test which measures the electrical activity in the heart. A number of electrodes (stickers) are put on the skin on your upper chest, arms, and legs. These are then connected to a monitor that records a snapshot or picture of how the heart is contracting. This test is used to look for any abnormal electrical activity in the heart. Watch
Exercise Stress Test: The exercise stress test is done while the individual walks or runs on a treadmill while connected to the EKG machine (see EKG). The test determines how the heart responds to exercise. Watch
Gene/Genetic: A gene is a segment of DNA which determines how the cells of the body function. Genes determine everything from an individual’s hair color to height. The alteration of a gene is called a genetic mutation. Watch
Holter Monitor: A Holter monitor is a portable form of an EKG that keeps track of an individual’s heartbeat. An individual will usually have to wear a Holter monitor for 24-48 hours. Watch
Implantable Cardioverter Defibrillator (ICD): The ICD is a device put under the skin that tracks the heartbeat and can deliver a shock to correct the heartbeat if an irregular heartbeat occurs.Watch
Pacemaker: Pacemakers are devices that are implanted under the skin. The pacemaker has wires that connect to the heart. A pacemaker can detect an abnormal heart beat and then send an electrical impulse to correct it. Watch
Seizure: A neurologic event due to abnormal electrical activity in the brain. Seizures can range from affecting a single body part to affecting the whole body. Watch
What is Marfan Syndrome?
Marfan syndrome is a condition caused by abnormal fibers within the tissues of the body. The abnormal tissues can be found in the aorta, which can start to bulge and become enlarged, which is known as an aneurysm. This can lead to the aorta tearing or breaking completely. The valves of the left side of the heart can also be affected. Both the aortic valve (which sits between the left ventricle and the aorta) and the mitral valve (which sits between the left atrium and left ventricle) are also affected by the abnormal fibers, causing them to become weak and unable to stand up to the pressures put on them by blood flowing through the heart. The aortic valve may also be stretched apart due to the enlarged aorta. This leads to blood flowing backwards into the heart from the aorta.
What are the symptoms of Marfan Syndrome?
People with Marfan syndrome are usually very tall, with long arms, legs, fingers, and toes. They may have a curved back and flexible joints and they may have problems with vision. People may have the following symptoms:
- Fatigue
- Shortness of breath
- Heart palpitations
- Chest pain (that can be felt in the back as well)
How is Marfan Syndrome diagnosed?
Marfan syndrome is usually diagnosed by a combination of your presenting symptoms and family history.
How is Marfan Syndrome treated?
There is no treatment for Marfan syndrome. The symptoms of Marfan syndrome are treated individually as they present. Regular visits to the cardiologist are needed to monitor the aorta and heart valves for any problems that may arise. Medications may be used to prevent high blood pressure and irregular heartbeats. If the aorta or heart valves become extensively damaged, surgery is necessary to fix the problem.
MARFAN SYNDROME: IMPORTANT TERMINOLOGY
Atrium (Atria pl.): The upper chambers of the heart. There are two atria: left and right.
Aorta: The great artery arising from the left ventricle of the heart; the largest artery in the human body.
Aortic valve: The three-leafed valve that separates the left ventricle from the aorta.
Echocardiogram: An echocardiogram is a type of ultrasound test that is used to look at the structure of the heart. The sonographer will move a transducer, with cool gel on it, across your chest and upper ribs. The transducer uses painless sound waves to look at the structure of the heart. Watch
Electrocardiogram (EKG or ECG): An electrocardiogram is a test that measures the electrical activity in the heart. A number of electrodes (stickers) are put on the skin on your upper chest, arms, and legs. These are then connected to a monitor that records a snapshot or picture of how the heart is contracting. This test is used to look for any abnormal electrical activity in the heart. Watch
Genetic Mutation: A genetic mutation is a change in an individual’s DNA which can lead to improper functioning of their body’s cells. These mutations or changes may be passed down through generations. Watch
Mitral valve: The two-leafed valve that separates the left atrium from the left ventricle.
Ventricle (Ventricles pl.): The lower chambers of the heart. There are two ventricles: left and right.
What is Mitral Valve Prolapse?
Mitral Valve Prolapse (MVP), present in about 2% of the population, is a condition in which one of the valves of the heart doesn’t close properly. This defect allows blood to flow backward through the heart. This backward flow can cause damage to the heart and decreases its ability to pump blood to the body. MVP can be a congenital disease and can occur in families or in individuals with no prior family history. The condition develops gradually as the leak increases.
MVP can lead to infections of the heart valves, strokes or abnormal heart rhythms over time. Watch
What are symptoms of Mitral Valve Prolapse?
There are a number of symptoms that may occur with Mitral Valve Prolapse. These symptoms include:
- Rapid heartbeat (Palpitations)
- Trouble breathing
- Dizziness
- Numbness
- Tingling
- Passing out spells [Fainting (Syncope)]
- Chest pain
- Anxiety disorders
An individual should consult a healthcare professional if any of these symptoms are present.
How is Mitral Valve Prolapse Diagnosed?
There are certain signs and symptoms that may be present with MVP. The physician will check for a heart murmur (extra or abnormal sound) when listening to your heart. Some tests to diagnose MVP may include an Electrocardiogram (EKG) or Echocardiogram.
How is MVP Treated?
Those who have Mitral Valve Prolapse but don’t have symptoms may not need treatment. Many patients appear to benefit from a change in lifestyle, including aerobic exercise training and avoidance of stimulants (caffeine), alcohol, and undue fatigue. Individuals with MVP may also benefit from stress reduction. If you have symptoms your doctor may prescribe certain medications:
- Beta blockers– These medications slow your heart down
- Diuretics- These medications decrease the load on the heart. They may make individuals go to the bathroom frequently.
- Heart rhythm medications- These medication prevent the heart from going into an abnormal rhythm
- Blood thinning medications- These medications decrease the load on the heart. Individuals on blood thinning medication may experience easy bleeding or bruising.
Magnesium is a medication which may help with some symptoms, especially chest pain.
MITRAL VALVE PROLAPSE: IMPORTANT TERMINOLOGY
Cardiovascular MRI (CV MRI): The CV MRI looks at the structure of the heart to identify any abnormalities. Watch
Congenital Disease: Congenital refers to a condition diagnosed at birth.
Echocardiogram: An echocardiogram is a type of ultrasound test that is used to look at the structure of the heart. The sonographer will move a transducer, with cool gel on it, across your chest and upper ribs. The transducer uses painless sound waves to look at the structure of the heart. Watch
Electrocardiogram (EKG or ECG): An electrocardiogram is a test that measures the electrical activity in the heart. A number of electrodes (stickers) are put on the skin on your upper chest, arms, and legs. These are then connected to a monitor that records a snapshot or picture of how the heart is contracting. This test is used to look for any abnormal electrical activity in the heart. Watch
Valve: The heart has valves that direct blood flow through its chambers (the atria and ventricles). The valves open to let blood through and close to prevent blood from moving backward.
What is myocarditis?
Myocarditis is an inflammation of the heart. Usually viruses cause myocarditis, but other factors can also contribute including bacteria, toxins, or autoimmune processes. Myocarditis may go away on its own, but sometimes it can lead to more serious issues, such as dilated cardiomyopathy and arrhythmias.
What are the symptoms of myocarditis?
Symptoms of myocarditis include the following:
- Tiredness
- Chest pain
- A feeling that the heart is skipping a beat
- Swelling of the legs and feet (edema)
- Trouble breathing
How is myocarditis diagnosed?
Diagnosis of myocarditis is made by a combination of presenting symptoms and lab tests, which will show the doctor that the heart has been damaged and is currently inflamed. An EKG can also show whether there is an arrhythmia. Your doctor may also do imaging studies like a chest x-ray, MRI, echocardiogram, or cardiac catheterization.
How is myocarditis treated?
Myocarditis is treated depending on the cause. Usually, medicines are given to help the patient’s heart beat properly, decrease inflammation, and keep fluid from building up. Rest and oxygen may be required as well until the myocarditis is gone.
MYOCARDITIS: IMPORTANT TERMINOLOGY
Cardiac catheterization: A procedure to look at the heart more closely. During this procedure, a tube is placed through the patient’s arm into the blood vessel and advanced to the heart. Once in place, the doctor puts dye through the tube into the heart that shows up on x-ray. This lets the doctor see how the chambers, valves, and arteries of the heart are working.
Echocardiogram: An echocardiogram is a type of ultrasound test that is used to look at the structure of the heart. The sonographer will move a transducer, with cool gel on it, across your chest and upper ribs. The transducer uses painless sound waves to look at the structure of the heart. Watch
Electrocardiogram (EKG or ECG): An electrocardiogram is a test that measures the electrical activity in the heart. A number of electrodes (stickers) are put on the skin on your upper chest, arms, and legs. These are then connected to a monitor that records a snapshot or picture of how the heart is contracting. This test is used to look for any abnormal electrical activity in the heart. Watch
What is SVT?
SVT is a condition that causes an abnormal electric current in the heart. This abnormal current can cause the heart to beat abnormally fast. This can last from a few minutes to a few hours. The symptoms may come on at rest or when an individual exercises or moves around.
What are symptoms of SVT?
The fast heartbeat can cause some of the following symptoms:
- Feelings that your heart is racing
- Episodes of passing out
- Lightheadedness or dizziness
- Excessive sweating
- Chest pain
- Shortness of breath
How is SVT diagnosed?
A physician will look for signs of SVT on the physical exam. They will feel your pulse to see if the heart is beating fast. The most important test for SVT is the Electrocardiogram or EKG. The EKG will help diagnose SVT as well as to determine which type of SVT. A Holter monitor may be used to record the heart’s electrical activity for a longer period of time.
How is SVT Treated?
The treatment for SVT focuses on fixing the electrical abnormality. There are a variety of treatments which include:
- Certain medications
- Cardioversion
- Ablation
Medications can help fix the unusual rhythm. If the medications don’t work, cardioversion may be attempted. If these approaches don’t work then a surgical procedure, called an ablation, may be performed.
SVT: IMPORTANT TERMINOLOGY
Ablation: A surgical procedure to correct an abnormal heart rhythm. The goal is to remove or destroy the region of the heart where the abnormal rhythm is originating from. Watch
Cardioversion: A mild electric current to correct an abnormal heart rhythm. The procedure involves placing a pad on the patient’s bare chest which senses the abnormal electric current and applies a mild electric shock to correct it. Patients are usually sedated so that they don’t feel the shock.
Electrocardiogram (EKG or ECG): An electrocardiogram is a test that measures the electrical activity in the heart. A number of electrodes (stickers) are put on the skin on your upper chest, arms, and legs. These are then connected to a monitor that records a snapshot or picture of how the heart is contracting. This test is used to look for any abnormal electrical activity in the heart. Watch
Holter Monitor: A Holter monitor is a portable EKG monitor which keeps track of your heartbeat. An individual will usually have to wear a Holter monitor for 24-48 hours. Watch
Paroxysmal: Symptoms that come suddenly and unexpectedly.
Supraventricular: This term refers to any abnormal electric current in the heart which starts in the upper chambers of the heart (atria).
Tachycardia: This term refers to a fast heartbeat. A fast heartbeat is one this greater 100 beats per minute. The heart rate can be measured by feeling a person’s pulse over a minute’s time.
What is WPW?
WPW is a problem with the electrical pathway of the heart. In a normal heart, a single electrical pathway goes from the atria, through the middle of the heart, and throughout the ventricles. In the middle of the heart, an area known as the AV node causes a pause in the circuit so that both the atria and the ventricles do not contract at the same time. This pause also keeps the ventricles from beating too fast if the atria become over excited. In WPW, however, an extra pathway, called an accessory pathway, goes along the outer wall of the heart. This specific accessory pathway is called the Bundle of Kent. When it is activated, electrical currents run through it to activate the ventricles of the heart early, causing an arrhythmia. In these patients, if the atria begin to beat abnormally fast, the electricity from them will not pause at the AV node, and instead go down the Bundle of Kent, causing the ventricles to beat abnormally fast as well.
What are the Symptoms of WPW?
WPW is usually asymptomatic. However, if the accessory pathway is activated, it can cause the person to have the following:
- A feeling that the heart is racing (palpitations)
- Dizziness
- Shortness of breath
- Lightheadedness or fainting spells
How is WPW diagnosed?
WPW is usually seen on an electrocardiogram or EKG. Some patients without symptoms who are at risk of having increased heart rate, such as athletes, may undergo electrophysiologic testing.
How is WPW treated?
If the patient does not have an issue with rapidly beating atria, there may be no need for treatment. In acute instances of arrhythmias, patients can perform maneuvers that can lower the heart rate by decreasing the amount of adrenaline in the body. These include bearing down (called the Valsalva maneuver) and massaging the main artery in the neck (called a carotid massage). These maneuvers will decrease the heart rate and potentially stop the arrhythmia. Patients with stronger symptoms can take medicine or undergo one of two procedures: radiofrequency ablation or surgery.
WOLFF PARKINSON WHITE: IMPORTANT TERMINOLOGY
Atrium (Atria pl.): The upper chambers of the heart. There are two atria: left and right.
Arrhythmia: An arrhythmia is abnormal heart beat. Some abnormal heartbeats are harmless while others can be dangerous. An arrhythmia is identified on an Electrocardiogram or EKG.
Electrocardiogram (EKG or ECG): An electrocardiogram is a test that measures the electrical activity in the heart. A number of electrodes (stickers) are put on the skin on your upper chest, arms, and legs. These are then connected to a monitor that records a snapshot or picture of how the heart is contracting. This test is used to look for any abnormal electrical activity in the heart. Watch
Electrophysiologic Testing: A procedure where the patient is sedated and small wires called electrode catheters are put into the thigh and run into the heart. These wires are able to accurately monitor the electrical pathways of the heart.
Radiofrequency Ablation: Performed during electrophysiologic testing, high frequency electricity is sent to the area where the abnormal electrical pathway is found, preventing it causing an abnormal heartbeat.
Ventricle (Ventricles pl.): The lower chambers of the heart. There are two ventricles: left and right.
To better understand terms related to your condition, you can check out our Glossary.
Get Involved
![]() Join us on Discord and learn more about how to spread the word about SCA prevention.
Join us on Discord and learn more about how to spread the word about SCA prevention.
Take the Prevention Promise and share our flyers, poster, videos and more with your community
Need help raising money for AEDs or other prevention activities? Ask us how!
Make sure your home, school, team and hangouts are ready to Call Push Shock in a cardiac emergency.
Lend your heart and hands to the hundreds of community heart screenings and CPR/AED training and placement iniatives to advance prevention.

